Thickened Liquids & Modified Foods
Clinical care of children and adolescents who require thickened liquids and/or modified food texture diets often due to dysphagia, aspiration, or aspiration risk
Dysphagia (difficulty swallowing) can lead to aspiration, malnutrition, dehydration, prolonged feeding disorders, and/or altered childhood development. Thickened liquids help prevent aspiration because they flow slower than thin liquids, which provides extra time for a child with dysphagia to achieve airway protection during swallowing. [Barbon: 2018] They can also decrease regurgitation and risk for aspiration of gastric contents. Effective liquid thickening can prevent the need for tube feedings in many children. Modified food texture diets can facilitate swallowing in children with impaired swallowing. In collaboration with feeding specialists, the medical home team may see many patients make gradual improvements or a full recovery, depending on the underlying cause.
Key Points
- Check for new safety concerns before prescribing a thickener. Many thickeners are not approved for infants.
- Children with dysphagia should work with a feeding therapist to improve swallowing skills, help manage liquid thickening and food texture modifications, and safely wean off thickening liquids as swallowing skills improve.
- Use standardized terms and instructions from the International Dysphagia Diet Standardisation Initiative Framework (IDDSI) (
 2.3 MB) to reduce
variability.
2.3 MB) to reduce
variability.
- Thickeners are typically well-tolerated and have few side effects, but they can contribute to dehydration and increase the caloric density of the liquid.
- Regular follow-up is needed to adjust total fluid intake, monitor growth, ensure thickeners are tolerated, and evaluate symptom improvement. [Duncan: 2019] [Cichero: 2013] Also, monitor for silent aspiration - often indicted by choking, gagging, vomiting, and recurrent pneumonitis or lower respiratory tract infections.
- Some thickened medications can lead to sub-therapeutic medication levels; Class III BCS drugs are particularly vulnerable. [Cichero: 2013] Consult a pharmacist for guidance if needed.
- High-quality evidence is lacking about thickeners for infants with reflux; however, expert opinion is that thickened feeds improve visible regurgitation but do not alter acid reflux assessed by pH probe. [Rosen: 2018]
Role of the Medical Home
Once a need for thickened fluids or a modified-texture diet has been identified (see Feeding & Swallowing Problems in Children), the primary care clinician will typically rely on a feeding therapist, often a speech-language pathologist, to develop recommendations for managing the child’s dysphagia. Recommendations may include position changes, external pacing strategies, bottle nipple or cup modifications, liquid thickening, and/or food texture modifications.
While thickeners are typically well-tolerated and have few side effects, close follow-up is needed to ensure patients tolerate thickeners and have adequate symptom improvement. [Duncan: 2019] Children are monitored for choking, gagging, vomiting, and recurrent pneumonitis or lower respiratory tract infections since these would be red flags for silent aspiration. Children are also closely monitored for oral aversion or feeding disorders, which can develop over time. It is important that a feeding therapist works with patients to improve swallowing skills and help manage liquid thickening and food texture modification.
After initiating or altering liquid thickener or feeding modifications, the feeding therapist can help the child safely wean off thickening liquids as swallowing skills improve. [Wolter: 2018] The primary care clinician and feeding therapist can collaborate regarding the timing of repeat modified barium swallow studies if needed. Clinicians are encouraged to prescribe the minimum thickness needed for swallowing safety and help the patient safely wean off thickeners when swallowing skills improve. [Wolter: 2018] [Cichero: 2013] The primary care clinician or subspecialist should also provide basic guidance for families who need a modified diet for their child as well as monitor for appropriate growth and medical problems, such as inadequate fluid volume intake, constipation, reflux, and delayed gastric emptying.
Thickening Liquids
Determining Level of Thickness
- Eating and drinking
- Secretion management
- Oral hygiene
- Sensory status
- Ability to accept food
- Amount of diversity in the diet
- Management of oral medications
- Caregiver’s behaviors while feeding their child.
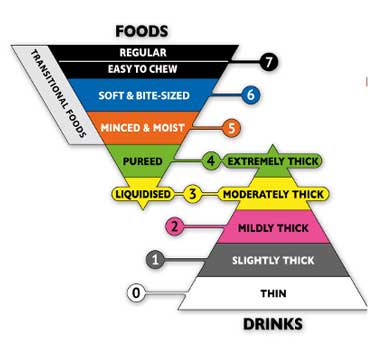
 2.3 MB) (left) standardized the
terminology describing food textures and liquid thicknesses to improve safety
for children with dysphagia. It consists of 8 levels (0 - 7), where drinks are
measured from Levels 0 – 4, and foods are measured from Levels 3 – 7. A gravity
flow test is used to find the liquid’s flow category, which uses a 10 mL slip
tip syringe and monitors the time it takes for the fluid to pass through. Simple
charts with images for each food texture and liquid thickness are available on
their website. It also includes descriptions and images for the syringe drip
test, fork spoon tilt, chopstick, and finger tests.
2.3 MB) (left) standardized the
terminology describing food textures and liquid thicknesses to improve safety
for children with dysphagia. It consists of 8 levels (0 - 7), where drinks are
measured from Levels 0 – 4, and foods are measured from Levels 3 – 7. A gravity
flow test is used to find the liquid’s flow category, which uses a 10 mL slip
tip syringe and monitors the time it takes for the fluid to pass through. Simple
charts with images for each food texture and liquid thickness are available on
their website. It also includes descriptions and images for the syringe drip
test, fork spoon tilt, chopstick, and finger tests.
Types of Thickeners
- Thickened formulas are commercially available. Benefits include a set viscosity; they may have improved digestibility and nutritional balance. They can be helpful for reflux; however, they tend to be only slightly thick, and often for dysphagia, an additional thickener is needed. [Salvatore: 2018]
- Food-based thickeners can displace formula volume and are typically recommended for thickening purees or solid foods rather than formula or breast milk. Banana, yogurt, pudding, blended foods, bread crumbs, crushed crackers, and infant cereal (see below) are examples of food-based thickeners.
- Infant cereal can be added to infant formula to reduce regurgitation. Breastmilk can break down infant cereal, and it does not stay thickened. If cereal is used to thicken feeds, an oat-based cereal is generally preferred over rice cereal due to concerns about the contamination of rice with arsenic. Thickening with infant cereal may lead to excessive weight gain and constipation.
- Carob bean (e.g., Gelmix) is not approved for preterm infants until they have reached a minimum weight of 6 pounds and at least 42 weeks post-menstrual (gestational) age.
- Corn starch (e.g., Thick-It, Thick & Easy, Resource Thickenup) is not approved for infants. It seems to take more powder to get desired thickness.
- Xanthan gum (e.g., Simply Thick, Nestle ThickenUp, Thick & Easy Clear) is not approved for preterm infants or infants <12 months of age due to concerns about necrotizing enterocolitis (NEC). [Beal: 2012] [Woods: 2012] Caution should be used for any child over age 1 with a history of necrotizing enterocolitis or altered bowel anatomy.
- Tapioca flour/starch is an effective thickening agent for recipes, such as homemade pudding, cookie dough, sauces, and gravies.
- Gelatin thickens as it cools and is more difficult to regulate for liquid swallowing.
- Pectin is commonly used to thicken jams, jellies, and preserves. It may cause constipation and increased gas production/distension because it is an undigested fiber.
Paying for Thickeners
Safety Concerns for Thickeners
Modified Foods
Some children with dysphagia and/or other pediatric feeding disorders may need modified-food texture diets, as they can have difficulty tolerating certain textures. Tongue thrusting, gagging, regurgitation, pocketing in the cheeks, and/or vomiting may indicate that the child is not tolerating their feeding and may have a feeding disorder requiring modified food texture.
Determining Level of Texture
- Soft and moist throughout
- Can be scooped or shaped on a plate
- Not sticky
- No separate thin liquids (i.e., sauces/juices do not leak or drip from food)
- Require minimal chewing; biting is not required
- Minced-sized pieces of food: No larger than 4mm in width and 15mm in length (adults); no larger than 2mm in width and 8mm in length (children)
- Small lumps may be visible and easily mashed with tongue
- Food can be easily mashed with a small amount of pressure from a fork
- Can be eaten with a fork or spoon
- Can be scooped onto a fork without liquid dripping or crumbles falling off
Types of Thickened Foods
Specialty Collaborations & Other Services
Speech - Language Pathologists
(see RI providers
[34]) and
Occupational Therapy
(see RI providers
[22])
Refer to a feeding therapist, speech-language pathologist, or
occupational therapist with pediatric feeding and swallowing experience, education,
and training to evaluate and help treat dysphagia and pediatric feeding disorders
and guide thickened liquids and modified-food texture diets.
Pediatric Gastroenterology
(see RI providers
[18]),
Pediatric Pulmonology
(see RI providers
[6]), and
Pediatric Otolaryngology (ENT)
(see RI providers
[7])
Consult a pediatric gastroenterologist to assess a child's need for
nutritional evaluation and possible tube feeding, malabsorption concerns, esophageal
disorders, and other related medical issues. Pediatric pulmonology and ENT
specialists may offer further diagnostic tests (such as endoscopy) and treatment.
Dieticians and Nutritionists
(see RI providers
[3])
Refer to a dietitian/nutritionist to help adjust dietary intake for
proper nutrition.
Resources
Information & Support
Related Material on the Medical Home Portal
For Parents and Patients
How and Why to Thicken Liquids (Nationwide Children's)
How to thicken liquids with Similac, Gerber, Elecare, Enfamil, Neocate, Bright Beginnings, Boost, Pediasure, and other formulas.
Practice Guidelines
Lock J, La Via MC.
Practice parameter for the assessment and treatment of children and adolescents with eating disorders.
J Am Acad Child Adolesc Psychiatry.
2015;54(5):412-25.
PubMed abstract
This practice parameter from the American Academy of Child and Adolescent Psychiatry reviews evidence-based practices for
the evaluation and treatment of eating disorders in children and adolescents.
Rosen DS.
Identification and management of eating disorders in children and adolescents.
Pediatrics.
2010;126(6):1240-53.
PubMed abstract
This AAP clinical report includes a discussion of diagnostic criteria and outlines the initial evaluation, treatment including
pharmacotherapy, and monitoring of the patient with disordered eating. Reaffirmed Feb 2018
Rosen R, Vandenplas Y, Singendonk M, Cabana M, DiLorenzo C, Gottrand F, Gupta S, Langendam M, Staiano A, Thapar N, Tipnis
N, Tabbers M.
Pediatric Gastroesophageal Reflux Clinical Practice Guidelines: Joint Recommendations of the North American Society for Pediatric
Gastroenterology, Hepatology, and Nutrition and the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition.
J Pediatr Gastroenterol Nutr.
2018;66(3):516-554.
PubMed abstract / Full Text
Patient Education
Let's Talk About... Dysphagia (Spanish & English)
Printable, 2-page, patient education about diagnosis and management of dysphagia in children; Intermountain Healthcare.
Thickening Liquids and Pureeing Foods (IDDSI) ( 784 KB)
784 KB)
Two-page patient handouts about food characteristics to embrace and avoid when striving to achieve consistent food texture
level; International Dysphagia Diet Standardisation Initiative.
Tools
International Dysphagia Diet Standardisation Initiative Framework (IDDSI) ( 2.3 MB)
2.3 MB)
A continuum of 8 levels (0-7) of food levels of thickness; International Dysphagia Diet Standardisation Initiative.
Services for Patients & Families in Rhode Island (RI)
| Service Categories | # of providers* in: | RI | NW | Other states (3) (show) | | NM | NV | UT |
|---|---|---|---|---|---|---|---|---|
| Dieticians and Nutritionists | 3 | 1 | 1 | 4 | 6 | |||
| Feeding & Swallowing Disorders | 1 | 2 | 2 | 3 | ||||
| Occupational Therapy | 22 | 1 | 17 | 22 | 37 | |||
| Pediatric Gastroenterology | 18 | 2 | 5 | 2 | ||||
| Pediatric Otolaryngology (ENT) | 7 | 1 | 11 | 5 | 10 | |||
| Pediatric Pulmonology | 6 | 4 | 4 | 3 | ||||
| Speech - Language Pathologists | 34 | 4 | 23 | 11 | 65 | |||
| Swallow Study | 1 | 1 | ||||||
For services not listed above, browse our Services categories or search our database.
* number of provider listings may vary by how states categorize services, whether providers are listed by organization or individual, how services are organized in the state, and other factors; Nationwide (NW) providers are generally limited to web-based services, provider locator services, and organizations that serve children from across the nation.
Helpful Articles
Brooks L, Liao J, Ford J, Harmon S, Breedveld V.
Thickened Liquids Using Pureed Foods for Children with Dysphagia: IDDSI and Rheology Measurements.
Dysphagia.
2021.
PubMed abstract
Preparing thickened liquids with commercially available thickeners can result in poor compliance due to concerns regarding
taste, texture, accessibility, cost, thickness variability, and potential negative impact of these substances on a child's
immature digestive tract. The purpose of this study was to determine if liquids could be successfully thickened with widely
available, commercial pureed foods, and to assess how these mixtures compare to starch and gum-based thickening agents.
Duncan DR, Larson K, Rosen RL.
Clinical Aspects of Thickeners for Pediatric Gastroesophageal Reflux and Oropharyngeal Dysphagia.
Curr Gastroenterol Rep.
2019;21(7):30.
PubMed abstract
The purpose of this review is to discuss current knowledge and recent findings regarding clinical aspects of thickeners for
pediatric gastroesophageal reflux and oropharyngeal dysphagia. We review evidence for thickener efficacy, discuss types of
thickeners, practical considerations when using various thickeners, and risks and benefits of thickener use in pediatrics.
Oparaji JA, Sferra T, Sankararaman S.
Basics of Blenderized Tube Feeds: A Primer for Pediatric Primary Care Clinicians.
Gastroenterology Res.
2019;12(3):111-114.
PubMed abstract / Full Text
Authors & Reviewers
| Authors: | Kathryn Murray, MD |
| Kimberly P. Hirte, MA CCC-SLP | |
| Contributing Author: | Anna Ermarth, MD, MS |
| Reviewer: | Michelle Guttenplan, MBA, MEd CCC-SLP, CLT |
Page Bibliography
American Dietetic Association.
National dysphagia diet: Standardization for optimal care.
National Dysphagia Diet Task Force, and American Dietetic Association;
2002.
Barbon CEA, Steele CM.
Thickened Liquids for Dysphagia Management: a Current Review of the Measurement of Liquid Flow.
Curr Phys Med Rehabil Rep.
2018;6(4):220-226.
PubMed abstract / Full Text
Beal J, Silverman B, Bellant J, Young TE, Klontz K.
Late onset necrotizing enterocolitis in infants following use of a xanthan gum-containing thickening agent.
J Pediatr.
2012;161(2):354-6.
PubMed abstract
Brooks L, Liao J, Ford J, Harmon S, Breedveld V.
Thickened Liquids Using Pureed Foods for Children with Dysphagia: IDDSI and Rheology Measurements.
Dysphagia.
2021.
PubMed abstract
Preparing thickened liquids with commercially available thickeners can result in poor compliance due to concerns regarding
taste, texture, accessibility, cost, thickness variability, and potential negative impact of these substances on a child's
immature digestive tract. The purpose of this study was to determine if liquids could be successfully thickened with widely
available, commercial pureed foods, and to assess how these mixtures compare to starch and gum-based thickening agents.
Cichero JA.
Thickening agents used for dysphagia management: effect on bioavailability of water, medication and feelings of satiety.
Nutr J.
2013;12:54.
PubMed abstract / Full Text
Duncan DR, Larson K, Rosen RL.
Clinical Aspects of Thickeners for Pediatric Gastroesophageal Reflux and Oropharyngeal Dysphagia.
Curr Gastroenterol Rep.
2019;21(7):30.
PubMed abstract
The purpose of this review is to discuss current knowledge and recent findings regarding clinical aspects of thickeners for
pediatric gastroesophageal reflux and oropharyngeal dysphagia. We review evidence for thickener efficacy, discuss types of
thickeners, practical considerations when using various thickeners, and risks and benefits of thickener use in pediatrics.
Lock J, La Via MC.
Practice parameter for the assessment and treatment of children and adolescents with eating disorders.
J Am Acad Child Adolesc Psychiatry.
2015;54(5):412-25.
PubMed abstract
This practice parameter from the American Academy of Child and Adolescent Psychiatry reviews evidence-based practices for
the evaluation and treatment of eating disorders in children and adolescents.
Oparaji JA, Sferra T, Sankararaman S.
Basics of Blenderized Tube Feeds: A Primer for Pediatric Primary Care Clinicians.
Gastroenterology Res.
2019;12(3):111-114.
PubMed abstract / Full Text
Rosen DS.
Identification and management of eating disorders in children and adolescents.
Pediatrics.
2010;126(6):1240-53.
PubMed abstract
This AAP clinical report includes a discussion of diagnostic criteria and outlines the initial evaluation, treatment including
pharmacotherapy, and monitoring of the patient with disordered eating. Reaffirmed Feb 2018
Rosen R, Vandenplas Y, Singendonk M, Cabana M, DiLorenzo C, Gottrand F, Gupta S, Langendam M, Staiano A, Thapar N, Tipnis
N, Tabbers M.
Pediatric Gastroesophageal Reflux Clinical Practice Guidelines: Joint Recommendations of the North American Society for Pediatric
Gastroenterology, Hepatology, and Nutrition and the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition.
J Pediatr Gastroenterol Nutr.
2018;66(3):516-554.
PubMed abstract / Full Text
Salvatore S, Savino F, Singendonk M, Tabbers M, Benninga MA, Staiano A, Vandenplas Y.
Thickened infant formula: What to know.
Nutrition.
2018;49:51-56.
PubMed abstract
This study aimed to provide an overview of the characteristics of thickened formulas to aid health care providers manage infants
with regurgitations.
Wolter NE, Hernandez K, Irace AL, Davidson K, Perez JA, Larson K, Rahbar R.
A Systematic Process for Weaning Children With Aspiration From Thickened Fluids.
JAMA Otolaryngol Head Neck Surg.
2018;144(1):51-56.
PubMed abstract / Full Text
Woods CW, Oliver T, Lewis K, Yang Q.
Development of necrotizing enterocolitis in premature infants receiving thickened feeds using SimplyThick®.
J Perinatol.
2012;32(2):150-2.
PubMed abstract


 Get Help in Rhode Island
Get Help in Rhode Island