Newborn Transition Care Guideline
On this Page
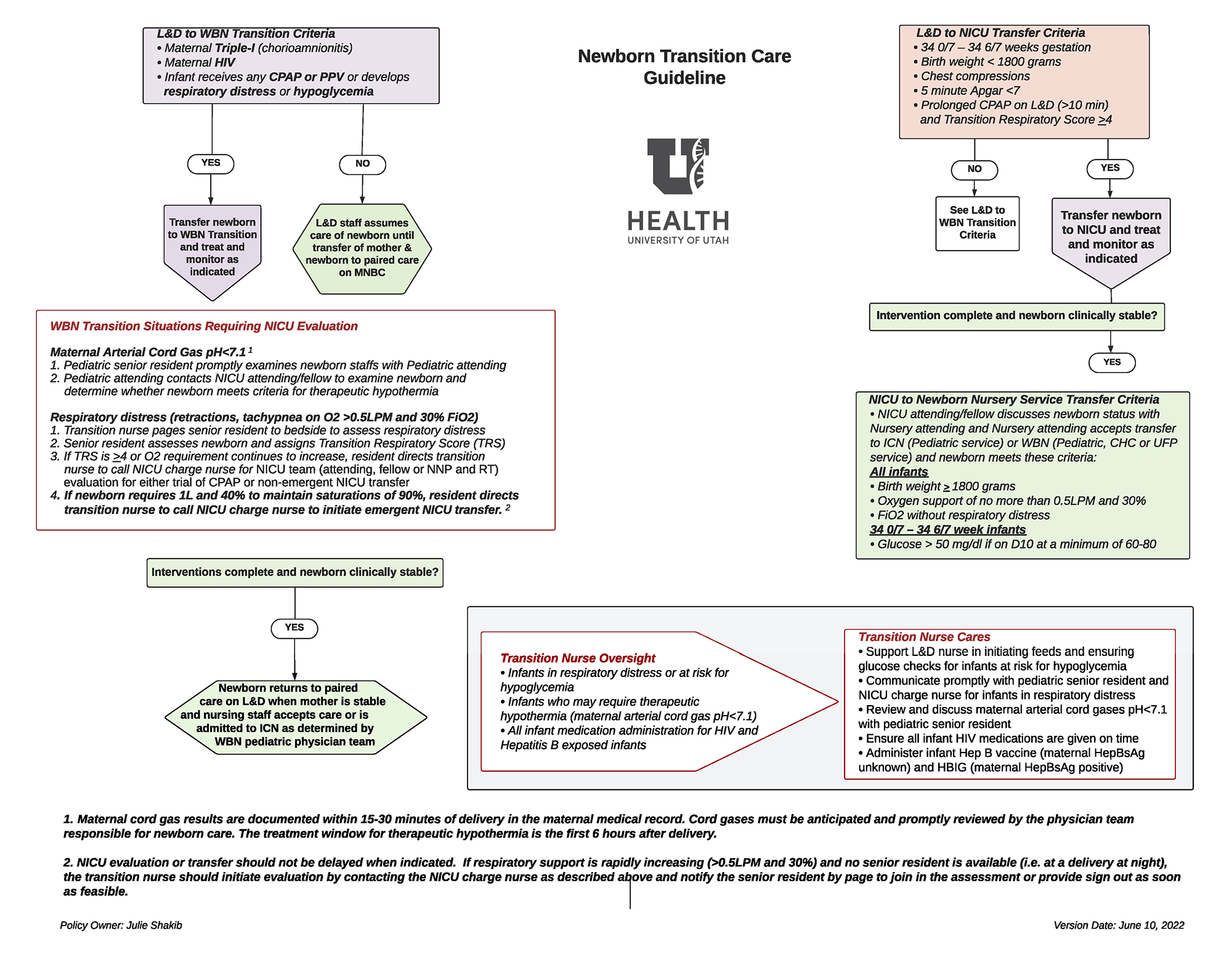
This care process model guides the University of Utah Hospital postpartum care team on the most appropriate level of care for the newborn directly after delivery. When medically appropriate, the preferred location for the newborn to transition is on the mother’s chest. Nonetheless, certain risk factors or concerning clinical findings should prompt the team to take the newborn either to the Well-Baby Nursery (WBN) Transition Area or to the Newborn Intensive Care Unit (NICU) for additional monitoring, support, and intervention.
Key Points
- Highest risk infants go directly to NICU after delivery: Infants with risk factors including prematurity <35 weeks, birth weight <1800 grams, receiving chest compressions, or prolonged CPAP and concerning respiratory status (e.g., a Transition Respiratory Score of >=4 at 10 minutes of life despite CPAP trial) should go to the NICU directly after delivery.
- Infants with moderate risk factors go to the WBN Transition Area after delivery: Infants with risk factors including maternal intrauterine infection (formerly referred to as chorioamnionitis) or maternal HIV, or having received any CPAP or PPV or with any respiratory distress or hypoglycemia who do not meet additional criteria for NICU care should transfer to the WBN Transition Area for monitoring to determine appropriate next level of care (e.g., NICU for escalating needs, Intermediate Care Nursery (ICN) for ongoing monitoring and moderate supports, or paired care with the mother in the WBN for stable, healthy infants).
- Infants with Possible HIE need SARNAT scoring: Infants who are found to have maternal arterial cord gas pH <7.15, 10-minute Apgar <6, maternal cord gas <7.15, or base deficit > 10 should be evaluated for risk of hypoxic-ischemic encephalopathy (HIE) by the NICU at 1-2 hours of life. Their SARNAT score determines the appropriate next steps of care.
- Infants with moderate care needs may transfer from the NICU to ICN or WBN: Infants who are in the NICU with a birth weight >=1800 grams and are comfortable on low levels of oxygen by nasal cannula with <=0.5 LPM and 30% FiO2 and stable glucoses may be accepted for care in the Intermediate Care Nursery (ICN. Stable infants >=35 0/7 weeks without the need for ongoing monitoring and support may go directly to the WBN for paired care. A transfer from the NICU to either ICN or the WBN requires an attending discussion.
- Stable infants with stable vitals and no ongoing need for interventions may be able to return to paired care on Labor and Delivery with adequate supervision.
Authors & Reviewers
Initial publication: February 2023
Current Authors and Reviewers:


 Get Help in Rhode Island
Get Help in Rhode Island