Postural Orthostatic Tachycardia Syndrome (POTS)
Guidance for primary care clinicians diagnosing and managing children with POTS
Postural orthostatic tachycardia syndrome (POTS) is a form of autonomic dysfunction with orthostatic intolerance that affects up to 1% of adolescents with chronic fatigue, dizziness, and, often, gastrointestinal discomfort or other forms of chronic pain. The prevalence of POTS has increased after COVID-19 with 2%-14% of COVID-19 survivors developing POTS and 9%-61% experiencing POTS-like symptoms. While evaluating tired, dizzy, uncomfortable adolescents, consider the diagnosis of postural orthostatic tachycardia syndrome and/or orthostatic intolerance and identify any relevant comorbidities. POTS is a real condition, even if it is a functional disorder with normal laboratory testing and imaging results. Most patients can fully recover and return to normal life activities with treatment.
POTS can be especially challenging for young athletes used to strenuous physical activity. Managing expectations in this particular population can go a long way in treatment and recovery.
Other Names
- Autonomic disorder or autonomic dysfunction (over-arching group of conditions of which POTS is a subset)
- Dysautonomia (same as autonomic dysfunction)
- Disorders of gut-brain interaction
- Orthostatic intolerance (broad group of problems characterized by bothersome symptoms when upright that improves when lying down; POTS is the form that is chronic and associated with excessive postural tachycardia)
- Postural tachycardia syndrome (preferred in Great Britain and abbreviated “PoTS”)
Key Points
Importance of diagnosis
Patients with chronic functional disability and a variety of
symptoms often seek lots of subspecialty care. With normal results of tests,
patients tend to keep seeking new doctors and new tests. It is vitally important
that an informed care provider coordinates the evaluation and management. With
an accurate diagnosis of POTS and appropriate treatment, unnecessary
consultation and "doctor shopping" can be avoided, and the focus on functional
restoration maintained.
Diagnosis criteria
The diagnosis of POTS is based on clinical history (>3 months of
daily intolerance of upright position) coupled with postural tachycardia (>40
beats per minute increase for patients 12-19 years and >30 beats per minute
increase for patients over 19 years) within 10 minutes of upright posture. See
Diagnosis below for specific criteria. Acute and intermittent symptoms do not
qualify for the diagnosis. Similar symptoms without excessive postural
tachycardia indicate orthostatic intolerance but not POTS. The treatment would
be identical to the treatment of POTS, except that medications are not needed
for orthostatic intolerance when there is no excessive postural tachycardia.
Please see Diagnosis section for detailed criteria.
Management of POTS symptoms
Advise patients to drink so much that their urine looks clear,
like water. Eat as much salt as tolerated; some patients prefer salt
tablets/capsules. Get aerobic exercise daily (working up to 30 minutes in a
single daily session). Get enough sleep every night and do not take naps. If
this is not possible, limit naps to once a day and no longer than 30 minutes -
avoid napping after 2 pm. Get help from a good psychologist and consider
medication, too. Please see Treatment and Management Section for more
information.
Importance of healthy lifestyle
Patients with POTS are further compromised when they get behind on
exercise, regular meals, sleep, and other healthy habits that help with stress
management and weight gain. They must keep their bodies in balance. With POTS,
maintaining academic and extra-curricular success (or even participation) is
difficult. Loving parents tend to do whatever they can to help the patient
succeed. However, individuals typically link 2 activities with their recovery –
staying in school and exercising regularly, the very activities that are most
challenging with POTS. A clear diagnosis and treatment plan help patients and
families support activity and recovery rather than inactivity and illness.
Parents need to facilitate normal activities rather than helping the patient to
stay comfortable with increasing debilitation.
Physical therapy
Working with a physical therapist who is knowledgeable in POTS can
be very beneficial. Also, adjusting expectations in athletes is important so
they do not set themselves up to fail by having high standards for physical
activity. If there is joint hypermobility, work with a physical therapist
familiar with hypermobility to teach patients how to strengthen and protect
their joints. Please see the Exercise Section below to find more details on an
Exercise Program for patients with POTS.
Importance of healthy nutrition
Iron deficiency and vitamin D deficiencies can worsen POTS
symptoms. A balanced diet and taking a daily multivitamin can be helpful.
Evaluating for nutritional deficiencies can help guide management if there are
concerns about poor diet. If iron deficiency is suspected, an actual treatment
dose would be indicated (daily multivitamins might not have enough iron to treat
iron deficiency).
Infections and POTS
Patients with POTS tend to get sicker with common illnesses than
others. Patients with POTS feel terrible in just about every way with just about
any symptom. It is vitally important that they adhere to and even exaggerate
their baseline fluid/salt intake and exercise/activity plan when they are
ill.
Failure to improve
Patients need to keep going forward, 1 little step at a time.
Failure to improve only rarely relates to medication. Here are things to
emphasize:
- Become more aggressive about increasing fluid and salt intake.
- Focus on daily aerobic exercise. If the person is too tired to exercise, find the amount of upright exercise the patient can do – even if just 2 minutes of light walking. Make the exercise intense enough so the patient breathes a bit faster than normal. Then, increase the duration of that daily exercise by 1-2 minutes every 5 days. Gradually, exercise tolerance will increase. Keep going until the patient can continue with 30 minutes of aerobic exercise daily.
- Participating in cognitive behavioral therapy is very important.
Family and friends supporting the recovery of normal function (as opposed to comfort with disability) is vital.
Practice Guidelines
Mostly because of a lack of comparative studies of treatment options, there are no official Practice Guidelines for POTS. Below is a summary of what is known so far about pediatric POTS:
Boris JR, Moak JP.
Pediatric Postural Orthostatic Tachycardia Syndrome: Where We Stand.
Pediatrics.
2022;150(1).
PubMed abstract / Full Text
See Helpful Articles in the Resources section for supportive literature.
Diagnosis
- Sustained heart rate increase of ≥ 30 beats/min (or ≥ 40 beats/min if patient is 12–19 yr within 10 minutes of upright posture.
- Absence of significant orthostatic hypotension (blood pressure drop ≥ 20/10 mm Hg).
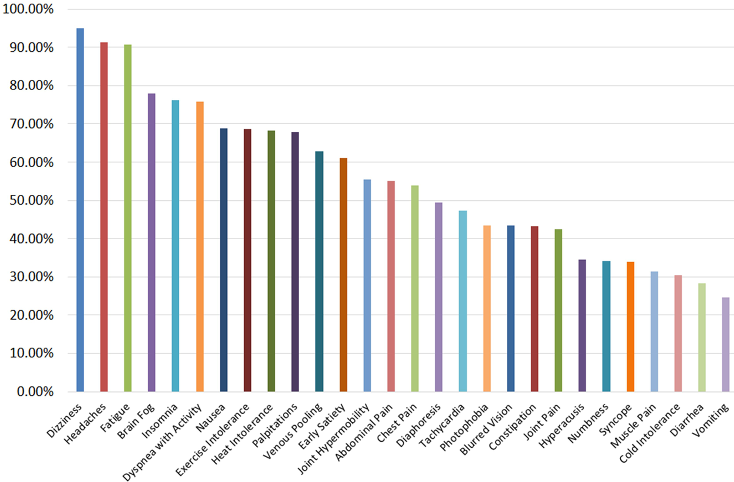
- Very frequent symptoms of orthostatic intolerance that are worse while upright, with rapid improvement upon return to a supine position. Symptoms vary among individuals but often include lightheadedness, palpitations, tremulousness, generalized weakness, blurred vision, and fatigue.
- Symptom duration ≥ 3 months.
- Absence of other conditions that could explain sinus tachycardia on standing
- Acute hypovolemia (from dehydration or blood loss)
- Anemia
- Orthostatic hypotension
- Endocrinopathy
- Adrenal insufficiency
- Carcinoid tumor
- Hyperthyroidism
- Pheochromocytoma
- Adverse effects from medication or polypharmacy.
- Panic attacks and severe anxiety
- Prolonged or sustained bed rest
- Recreational drug effects
History
- What are your biggest concerns?
- When do you remember being completely healthy?
- What was the first thing that affected you? Any inciting event?
- Any aggravating/relieving factors?
- What have you tried so far? What has worked?
- What top 3 things would you like to be doing that you can't do right now?
- How long can you stand, exercise?
- Does heat bother you?
- How do you feel after large meals?
- Do you sweat like others?
- Any changes to bowel movements? Any trouble digesting food?
- Any changes to sexual life/function?
- Any urinary concerns?
Family History
Presentations
Patients have upright dizziness and feel better lying down. Sometimes, they also have other upright symptoms (headache, heaviness, fatigue, cloudy thinking) partially abated by lying down. Patients can experience blurred vision when dizzy. Sometimes, these patients can be pre-syncopal or syncopal.
Almost all POTS patients have had bothersome fatigue for at least 3 months.
Orthostatic hypotension sometimes develops after postural tachycardia when upright. If the systolic blood pressure drops more than 20 mm Hg and/or the diastolic pressure drops >10 mmHg within the first 3 min of upright position, prior to an increase in heart rate, the problem is orthostatic hypotension rather than POTS. One way or the other, patients with POTS sometimes faint.
Most POTS patients have at least some gastrointestinal distress, like irritable bowel syndrome and nausea (functional gastrointestinal disorder). Of course, before assuming that POTS is the cause, celiac disease and inflammatory bowel disease should be considered.
Many patients with POTS have irregular temperature regulation, such as “wilting” outside on hot days, requiring different numbers of layers of clothes than peers, or sensing low-grade fevers.
Many POTS patients feel like they cannot think clearly or remember things. It is unclear whether this relates to altered cerebral blood flow or altered chemical activation of brain cells. However, cognitive testing does not usually reveal measurable deficits.
Diagnostic Criteria and Classifications
Genetics & Inheritance
Screening & Diagnostic Testing
Genetics & Inheritance
Prevalence
Differential Diagnosis
Co-Occurring Conditions
- Iron deficiency: Nearly ½ of patients with POTS have ferritin levels <20 ng/dL and benefit some from iron supplementation.
- Vitamin D deficiency: About ⅓ of POTS patients have 25-OH-vitamin D levels <20 ng/dL and benefit to some degree from vitamin D supplementation.
- Anxiety and depression: Approximately ⅓ of patients with POTS have significant anxiety and/or depression, some of which preceded the onset of POTS symptoms. Similar neurotransmitters are involved in the regulation of both the autonomic nervous system and mood, which may be a factor. Chronic debilitation due to POTS could also trigger depression.
- Headache and other forms of chronic pain: Seen in the majority of those with POTS
- Motion sickness: Also common in POTS
Prognosis
There are limited data about the outcomes of adolescent-onset POTS. A study including adolescents and adults found that approximately 37% no longer had POTS 1 year after starting treatment.[Kimpinski: 2012] A study of adolescents surveyed about 1½ years after starting treatment found that most were significantly improved, especially those treated with beta-blockers. [Lai: 2009] A longer (average 5 years) follow-up survey of adolescents with POTS demonstrated that symptoms of POTS were resolved or markedly reduced in about 86% of respondents. [Bhatia: 2016] Even a vast majority of adolescents with POTS and/or debilitating chronic pain can return to normal activities within months of completing an intensive recovery program. [Bruce: 2017] While not all adolescents with POTS fully recover, optimism for a good recovery for most affected patients is warranted.
Treatment & Management
Instruct patients to increase fluid and salt intake, exercise daily, get adequate sleep, and engage in cognitive behavioral therapy techniques. Prescription medications are most useful when the patient fully engages in non-pharmacologic treatment modalities. [Lai: 2009]
In 1 study, nearly 90% recovered or greatly improved over a few years. However, some patients do not fully recover. [Bhatia: 2016] Management of individuals with POTS requires patience, persistence, and positivity.
Non-pharmacologic treatment (fluids, salt, exercise, compression garments, elevating the head of bed, therapy) may be sufficient and should be used for all patients.
Pharmacologic treatment (fludrocortisone, beta-blockers, antidepressants) may be very helpful for select patients. Most of those needing medications can discontinue them after 1-3 years. Helping the patient and the family understand the condition, implement and maintain needed lifestyle and dietary changes, and sustain optimism and goals for the future are key. For management of many patients with POTS, a physician familiar with the condition and a psychologist skilled in cognitive behavioral therapy are the only specialists needed. If the primary care provider or medical home physician is unfamiliar with POTS, a POTS-aware physician can help – be that a generalist, a neurologist, or a cardiologist. Some patients are more likely to continue daily exercise if they have a physical therapist or coach involved. Some institutions have multi-disciplinary teams for POTS so patients can see a POTS-aware physician, a psychologist, and a physical therapist on the same day. It prevents repeated hospital visits and bills and allows for care coordination.
Approach to
Treatment of POTS ( Figure 2 from Postural orthostatic
tachycardia syndrome: a clinical review
[Johnson: 2010]
Click image to access the abstract - article requires a subscription
to Pediatric Neurology.)
Table 2 from Pediatric
disorders of orthostatic intolerance
[Stewart: 2018]
Click image for free access to table.
- Fluids: Fluid intake goal- 3-4L per day- about 100-120 ounces
- Salt: Salt intake goal- 3-4 Grams sodium/day. Do not worry about the patient taking in too much salt unless diagnosed with hypertension. Most patients do not get enough salt, so optimizing that is very important.
- Compression garments are helpful, too, especially waist-high compression leggings. They help prevent pooling in the legs and abdomen. The goal is to achieve 20-30 mm Hg. Some brands that have carried compression wear from time to time are Under Armour, Second Skin, Old Navy, SPANK, Lululemon, CEP compression.com, Therafirm, and Bauerfeind.
-
Exercise: Adaptation to fatigue and other symptoms of POTS often
leads to deconditioning, which requires reconditioning exercise to
reverse. Find the amount of upright exercise the patient can do – even
if just 2 minutes of light walking. Make the exercise intense enough to
gradually increase tolerance, aiming for at least 30-60 minutes of
aerobic exercise every day. Sometimes, patients comply better with
exercise regimens if followed and guided by a physical therapist. The
POTS Exercise Program (CHOP) (
 1.4 MB) is
a unique exercise training program by the Children's Hospital of
Philadelphia designed for patients with POTS patients that starts with
exercise in a recumbent position.
1.4 MB) is
a unique exercise training program by the Children's Hospital of
Philadelphia designed for patients with POTS patients that starts with
exercise in a recumbent position.
- Elevate the head of the bed to reduce nocturnal diuresis and POTS symptoms.
Mental Health / Behavior
Medication
- Limit beta-blockers if there is excessive resting bradycardia.
- Absent excessive postural tachycardia, medications may not be indicated for orthostatic intolerance.
- If the patient still has excessive postural tachycardia an hour after taking a beta-blocker dose, the dose could be increased.
- Beta-blockers can cause rare worsening of asthma, rare difficulty recognizing symptoms of hypoglycemia in patients with diabetes, and occasional increased fatigue (especially with propranolol). Midodrine can cause a “creepy-crawly” sensation of the scalp with too high or too rapidly increasing a dose.
- Caffeine can stall recovery.
- Antihistamines might slightly hinder recovery, so they should only be used if truly needed.
Click image for free access to table.)
Table 2 from Pediatric disorders of orthostatic intolerance [Stewart: 2018]
Click image for free access to table.
Neurology
Gastro-Intestinal & Bowel Function
Nutrition
Endocrine/Metabolism
Cardiology
Musculoskeletal
Maturation/Sexual/Reproductive
Sleep
Education & School
Complementary & Alternative Medicine
Services & Referrals
For management of many patients with POTS, a physician who is familiar with the condition and a psychologist skilled in cognitive behavioral therapy are the only specialists needed. If the primary care provider or medical home physician is not familiar with POTS, the involvement of a POTS-aware physician can help – be that a generalist, a neurologist, or a cardiologist.
When to refer a patient with POTS
- No improvement noted with non-pharmacologic measures
- If the primary care clinician is not comfortable prescribing medications for POTS, or the patient does not improve with first-line medications like beta-blockers, or after targeting specific issues like anxiety and depression with SSRIs
- If symptoms are worsening
- If there are associated comorbidities complicating diagnostic picture and management
The Center for Autonomic Dysfunction and Research is a multi-disciplinary clinic for patients with POTS and dysautonomia. The team involves POTS-aware physicians, psychologists, and physical therapists.
Additional specialists can be helpful in the diagnosis and management of various aspects of care or comorbid conditions:
Pediatric Cardiology
(see RI providers
[17])
May be helpful in evaluation and management if sufficiently
experienced with POTS and to rule out concerning cardiac causes of syncope and
palpitations, if associated, or for specific cardiac concerns.
Pediatric Neurology
(see RI providers
[18])
May be helpful in evaluation if sufficiently experienced with POTS.
Physical Therapy
(see RI providers
[6])
May be helpful in designing and monitoring response to a
reconditioning program and for evaluation and management of excessive pain. Some
patients are more likely to continue daily exercise if they have a physical
therapist or coach involved.
Behavioral Therapies
(see RI providers
[32])
Referral for cognitive behavioral therapy (CBT) is likely appropriate
for all those diagnosed with POTS.
Individual Counseling
(see RI providers
[36])
Other mental health providers may be helpful for assessment and
treatment of depression and/or anxiety, or if no CBT providers are available.
Pediatric Integrative Medicine
(see RI providers
[0])
May be helpful to direct components of management, including
traditional and complementary modalities in a safe and evidence-based manner.
Pediatric Gastroenterology
(see RI providers
[18])
May be helpful in managing GI problems not responsive to primary care
measures.
ICD-10 Coding
G90. A is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. ICD-10-CM G90. A is a new 2023 ICD-10-CM code that became effective on October 1, 2022.
Resources
Information & Support
Related Portal Content
For Professionals
Postural Orthostatic Tachycardia Syndrome (GARD)
Includes information about symptoms, inheritance, diagnosis, finding a specialist, related diseases, and support organizations;
Genetic and Rare Diseases Information Center of the National Center for Advancing Translational Sciences.
Postural Orthostatic Tachycardia Syndrome - Grand Rounds Lecture
One-hour video of a Grand Rounds lecture at Primary Children's Hospital by Phillip Fischer, MD (2014), includes patient accounts
of the condition.
Patient Education
POTS (Postural Orthostatic Tachycardia Syndrome) (FAQ)
Answers to questions that families may have about
POTS.
Patient Education for POTS (Primary Children's Hospital) ( 239 KB)
239 KB)
Detailed recommendations for care of an adolescent with POTS or orthostatic intolerance.
Postural Tachycardia Syndrome (POTS) (Mayo Clinic)
Five-minute video for patients and families of Phil Fischer, MD (author of this module) explaining POTS.
Tools
Table of Medications to Manage POTS
Medication, Dosing, Side Effects, and comments; from Stewart JM, Boris JR, Chelimsky G, Fischer PR, Fortunato JE, Grubb BP,
Heyer GL, Jarjour IT, Medow MS, Numan MT, Pianosi PT, Singer W, Tarbell S, Chelimsky TC. Pediatric disorders of orthostatic
intolerance.
Pediatrics. 2018;141
Services for Patients & Families in Rhode Island (RI)
| Service Categories | # of providers* in: | RI | NW | Other states (3) (show) | | NM | NV | UT |
|---|---|---|---|---|---|---|---|---|
| Behavioral Therapies | 32 | 1 | 17 | 19 | 36 | |||
| Individual Counseling | 36 | 4 | 9 | |||||
| Pediatric Cardiology | 17 | 3 | 4 | 4 | ||||
| Pediatric Gastroenterology | 18 | 2 | 5 | 2 | ||||
| Pediatric Integrative Medicine | 1 | |||||||
| Pediatric Neurology | 18 | 5 | 5 | 8 | ||||
| Physical Therapy | 6 | 12 | 9 | 40 | ||||
For services not listed above, browse our Services categories or search our database.
* number of provider listings may vary by how states categorize services, whether providers are listed by organization or individual, how services are organized in the state, and other factors; Nationwide (NW) providers are generally limited to web-based services, provider locator services, and organizations that serve children from across the nation.
Studies
Clinical Studies of POTS (clincaltrials.gov)
Studies looking at better understanding, diagnosing, and treating this condition; from the National Library of Medicine.
Helpful Articles
Ormiston CK, Świątkiewicz I, Taub PR.
Postural orthostatic tachycardia syndrome as a sequela of COVID-19.
Heart Rhythm.
2022;19(11):1880-9.
PubMed abstract / Full Text
Raj SR, Fedorowski A, Sheldon RS.
Diagnosis and management of postural orthostatic tachycardia syndrome.
CMAJ.
2022;194(10):E378-E385.
PubMed abstract / Full Text
Rao P, Peritz DC, Systrom D, Lewine K, Cornwell WK 3rd, Hsu JJ.
Orthostatic and Exercise Intolerance in Recreational and Competitive Athletes With Long COVID.
JACC Case Rep.
2022;4(17):1119-1123.
PubMed abstract / Full Text
Bourne KM, Sheldon RS, Hall J, Lloyd M, Kogut K, Sheikh N, Jorge J, Ng J, Exner DV, Tyberg JV, Raj SR.
Compression Garment Reduces Orthostatic Tachycardia and Symptoms in Patients With Postural Orthostatic Tachycardia Syndrome.
J Am Coll Cardiol.
2021;77(3):285-296.
PubMed abstract
Cooper VL, Hainsworth R.
Head-up sleeping improves orthostatic tolerance in patients with syncope.
Clin Auton Res.
2008;18(6):318-24.
PubMed abstract
Tome J, Kamboj AK, Loftus CG.
Approach to Disorders of Gut-Brain Interaction.
Mayo Clin Proc.
2023;98(3):458-467.
PubMed abstract
Authors & Reviewers
| Author: | Kirti Sivakoti, MD |
| Reviewer: | Phil Fischer, MD |
| 2023: update: Kirti Sivakoti, MDA |
| 2020: revision: Gisela G. Chelimsky, MDR |
| 2019: first version: Phil Fischer, MDA |
Page Bibliography
Bhatia R, Kizilbash SJ, Ahrens SP, Killian JM, Kimmes SA, Knoebel EE, Muppa P, Weaver AL, Fischer PR.
Outcomes of Adolescent-Onset Postural Orthostatic Tachycardia Syndrome.
J Pediatr.
2016;173:149-53.
PubMed abstract
Over a few years, 86% or more of patients with adolescent-onset POTS report recovery or significant improvement.
Boris JR, Moak JP.
Pediatric Postural Orthostatic Tachycardia Syndrome: Where We Stand.
Pediatrics.
2022;150(1).
PubMed abstract / Full Text
Bourne KM, Sheldon RS, Hall J, Lloyd M, Kogut K, Sheikh N, Jorge J, Ng J, Exner DV, Tyberg JV, Raj SR.
Compression Garment Reduces Orthostatic Tachycardia and Symptoms in Patients With Postural Orthostatic Tachycardia Syndrome.
J Am Coll Cardiol.
2021;77(3):285-296.
PubMed abstract
Bruce BK, Weiss KE, Ale CM, Harrison TE, Fischer PR.
Development of an Interdisciplinary Pediatric Pain Rehabilitation Program: The First 1000 Consecutive Patients.
Mayo Clin Proc Innov Qual Outcomes.
2017;1(2):141-149.
PubMed abstract / Full Text
Cooper VL, Hainsworth R.
Head-up sleeping improves orthostatic tolerance in patients with syncope.
Clin Auton Res.
2008;18(6):318-24.
PubMed abstract
Ghandour RM, Overpeck MD, Huang ZJ, Kogan MD, Scheidt PC.
Headache, stomachache, backache, and morning fatigue among adolescent girls in the United States: associations with behavioral,
sociodemographic, and environmental factors.
Arch Pediatr Adolesc Med.
2004;158(8):797-803.
PubMed abstract
Johnson JN, Mack KJ, Kuntz NL, Brands CK, Porter CJ, Fischer PR.
Postural orthostatic tachycardia syndrome: a clinical review.
Pediatr Neurol.
2010;42(2):77-85.
PubMed abstract
Since this publication, the diagnostic criteria for adolescent POTS have been refined to include a postural tachycardia of
at least 40 beats per minute change (instead of 30, as for adults). The suggested non-pharmacologic and pharmacologic treatment
strategies remain the same.
Kimpinski K, Figueroa JJ, Singer W, Sletten DM, Iodice V, Sandroni P, Fischer PR, Opfer-Gehrking TL, Gehrking JA, Low PA.
A prospective, 1-year follow-up study of postural tachycardia syndrome.
Mayo Clin Proc.
2012;87(8):746-52.
PubMed abstract / Full Text
Lai CC, Fischer PR, Brands CK, Fisher JL, Porter CB, Driscoll SW, Graner KK.
Outcomes in adolescents with postural orthostatic tachycardia syndrome treated with midodrine and beta-blockers.
Pacing Clin Electrophysiol.
2009;32(2):234-8.
PubMed abstract
Even over the months of initial treatment, most patients receiving a beta-blocker improve and credit the medication with their
improvement.
Ojha A, Chelimsky TC, Chelimsky G.
Comorbidities in pediatric patients with postural orthostatic tachycardia syndrome.
J Pediatr.
2011;158(1):20-3.
PubMed abstract
Ormiston CK, Świątkiewicz I, Taub PR.
Postural orthostatic tachycardia syndrome as a sequela of COVID-19.
Heart Rhythm.
2022;19(11):1880-9.
PubMed abstract / Full Text
Raj SR, Fedorowski A, Sheldon RS.
Diagnosis and management of postural orthostatic tachycardia syndrome.
CMAJ.
2022;194(10):E378-E385.
PubMed abstract / Full Text
Rao P, Peritz DC, Systrom D, Lewine K, Cornwell WK 3rd, Hsu JJ.
Orthostatic and Exercise Intolerance in Recreational and Competitive Athletes With Long COVID.
JACC Case Rep.
2022;4(17):1119-1123.
PubMed abstract / Full Text
Rimes KA, Goodman R, Hotopf M, Wessely S, Meltzer H, Chalder T.
Incidence, prognosis, and risk factors for fatigue and chronic fatigue syndrome in adolescents: a prospective community study.
Pediatrics.
2007;119(3):e603-9.
PubMed abstract
Shaw BH, Stiles LE, Bourne K, Green EA, Shibao CA, Okamoto LE, Garland EM, Gamboa A, Diedrich A, Raj V, Sheldon RS, Biaggioni
I, Robertson D, Raj SR.
The face of postural tachycardia syndrome - insights from a large cross-sectional online community-based survey.
J Intern Med.
2019;286(4):438-448.
PubMed abstract / Full Text
Silverman MN, Heim CM, Nater UM, Marques AH, Sternberg EM.
Neuroendocrine and immune contributors to fatigue.
PM R.
2010;2(5):338-46.
PubMed abstract / Full Text
Stewart JM, Boris JR, Chelimsky G, Fischer PR, Fortunato JE, Grubb BP, Heyer GL, Jarjour IT, Medow MS, Numan MT, Pianosi PT,
Singer W, Tarbell S, Chelimsky TC.
Pediatric disorders of orthostatic intolerance.
Pediatrics.
2018;141(1).
PubMed abstract / Full Text
This paper reviews standard management of adolescents with POTS and also mentions non-standard treatments that only have anecdotal
support of efficacy.
Tarbell SE, Olufs EL, Fischer PR, Chelimsky G, Numan MT, Medow M, Abdallah H, Ahrens S, Boris JR, Butler IJ, Chelimsky TC,
Coleby C, Fortunato JE, Gavin R, Gilden J, Gonik R, Klaas K, Marsillio L, Marriott E, Pace LA, Pianosi P, Simpson P, Stewart
J, Van Waning N, Weese-Mayer DE.
Assessment of comorbid symptoms in pediatric autonomic dysfunction.
Clin Auton Res.
2023.
PubMed abstract
ter Wolbeek M, van Doornen LJ, Kavelaars A, Heijnen CJ.
Severe fatigue in adolescents: a common phenomenon?.
Pediatrics.
2006;117(6):e1078-86.
PubMed abstract
Tome J, Kamboj AK, Loftus CG.
Approach to Disorders of Gut-Brain Interaction.
Mayo Clin Proc.
2023;98(3):458-467.
PubMed abstract


 Get Help in Rhode Island
Get Help in Rhode Island